Facts do not cease to exist because they are ignored.
Aldous Huxley

Coronavirus stories are everywhere.
On my newsfeed, on the news, on my social media, in my emails.
Too many of these stories are wrong. At best they are merely misleading, at worst they could completely mess up the appropriate policy choices.
- The Story Problem
- Your Physician may not be an Epidemiologist
- Why did I decide to write this article?
- A few examples:
- What did the Chinese CDC learn about the early spread of COVID-19?
- How does COVID-19 disease progress?
- What have we learned since about how the virus spreads?
- How did we get to a global pandemic?
- Why testing is a tool in the fight, but an incomplete solution.
- The worst-case analysis should be for scientists and policymakers only.
- Real criminal COVID-19 behavior – reckless endangerment!
- What is the problem with the case examples given at the beginning?
- Conceptualizing the Strategy
- Why we need testing to get better fast.
- A Hidden Benefit?
- Lessons Learned
- Improvements needed for future
- Postscript
- Sources:
- Just A Detour…
The Story Problem
Stories are compelling. Statistics are boring.
In a battle between stories and statistics, stories always win.
They should not!
Stories are personal observations. Statistics are impersonal abstractions.
Stories are easy to understand. Statistics require a level of familiarity with mathematics, which is deficient in our society.
Our media, which already struggles with mathematical concepts, are attracted to the dramatic stories because of the potential click-bait.
Few will bother with the real statistics and their implications.
Stories are good for stirring up emotional responses, fear, panic, a call to action.
People remember stories much easier than they remember statistics or facts.
The availability heuristic is a mental shortcut that occurs when people make judgments about the probability of events on the basis of how easy it is to think of examples. The availability heuristic operates on the notion that, “if you can think of it, it must be important.”
Daniel Kahneman – Nobel Prize in Economics sciences, Author – Thinking, Fast and Slow
But stories are a terrible way to understand the reality of a situation and make policy decisions.
Policies based on stories, and which ignore statistics will cause harm.
Your Physician may not be an Epidemiologist
Your Physician is a professional, and well trained.
Most medical professionals including your Physician see stories. Many stories. Every day.
They are on the front line and we will need them to be successful to combat the virus.
But, Epidemiologists collect Physician stories into a collective experience of the health system to build statistically significant learnings.
Dr. Anthony Fauci and Dr. Deborah Birx, the faces of the medical profession among the US Government Task Force and trained to understand the difference between stories and statistics.
In this article, I want to deal with the statistics and facts surrounding Coronavirus rather than the stories and myths that abound.
I am not a medical professional, so for the medical aspects of the virus, I would refer you to coronavirus.gov or cdc.gov or your Physician.
Instead, I will deal with the epidemiology of this epidemic. That is because this field is easier to understand through a mathematical and statistical lens.
Why did I decide to write this article?
Well, quite frankly, I began seeing such misunderstanding and massive misinformation in my news feed so regularly that I became concerned.
A few examples:
On Thursday, March 12, after the President of the United States announced a temporary travel ban to Europe, a smart friend of mine writes the following on Facebook:
“I’m sorry, but this announced travel ban is ridiculous, arbitrary, and will be both punitive and ineffective. Sorry. Random action without a basis in science is both frustrating, damaging, and insufficient.”
Sunday, March 15 on MSNBC’s “AM Joy,” Washington Post opinion writer Jennifer Rubin said:
“There is a particular cruelty, irony that it is their core viewers, the Republican older viewers, who are the most at risk…”
So typically, there will be less Democrat deaths because there will be less mass gatherings…” [1]
She essentially argues there would be fewer Democrat coronavirus deaths because they are adhering to suggestions offered by experts and the media.
Friday, March 13, Cliff Mass, a competent scientist, and math/statistics savvy weather analysis guy, writes on his blog a piece titled: “Panic and the Coronavirus: is there a better approach.” [2] It’s a thoughtful piece until he gets to the debate on social distancing:
“The Extreme Cost of the Current “Social Distancing” Approach. Currently, the “social distancing” approach is being stressed by politicians and others…
You notice the number of cases doesn’t change (the area under the curve). And it has another issue: it greatly extends the period in which society is affected by the disease…
The cost of social distancing is immense, something many politicians do not seem to have thought through…
Something more effective is needed, something I would call “smart quarantine…”
I think it would be useful to test an alternative strategy, based mainly on testing those that are not ill, and removing those people from social interaction.”
I know you are saying that you don’t see what’s wrong with any of these.
I will get back to each of these and discuss them in more detail a little later.
But first, we need to lay some groundwork for how this virus behaves and then draw some conclusions.
What did the Chinese CDC learn about the early spread of COVID-19?
A novel coronavirus first appeared in Wuhan, China, a city of some 11 million people, most likely in mid-December 2019.
The Chinese Center for Disease Control and Prevention (commonly referred to as Disease Control China) recently released a study of the first 425 patients with Novel Coronavirus – Infected Pneumonia (NCIP, aka COVID-19). [3] They provide the first epidemiologic characteristics of the virus, as experienced in Wuhan. Here is what they surmised:
Among the first 425 patients with confirmed NCIP, the median age was 59 years, and 56% were male. The majority of cases (55%) with onset before January 1, 2020, were linked to the Huanan Seafood Wholesale Market, as compared with 8.6% of the subsequent cases. The mean incubation period was 5.2 days (95% confidence interval [CI], 4.1 to 7.0), with the 95th percentile of the distribution at 12.5 days. In its early stages, the epidemic doubled in size every 7.4 days. With a mean serial interval of 7.5 days (95% CI, 5.3 to 19), the basic reproductive number was estimated to be 2.2 (95% CI, 1.4 to 3.9).
And their conclusion:
On the basis of this information, there is evidence that human-to-human transmission has occurred among close contacts since the middle of December 2019. Considerable efforts to reduce transmission will be required to control outbreaks if similar dynamics apply elsewhere. Measures to prevent or reduce transmission should be implemented in populations at risk.
How does COVID-19 disease progress?
The plain language interpretation of the above study and additional learning is provided to us by Dr. Charles Chiu, MD, Ph.D., UC San Francisco Infectious Disease Expert: [4]
“Once a person is exposed and becomes infected, the incubation period before the onset of symptoms is about five days, although this can vary from two to 11 days. Flu-like symptoms are often mild at first and some patients recover without the symptoms becoming more serious. But for a subset who get worse, day four after the onset of symptoms is usually when they seek medical care because they develop shortness of breath and early pneumonia, and they may become critically ill by day seven. After day 11, most patients who survive are on their way to recovery.”
What have we learned since about how the virus spreads?
The USA CDC building on the early experience shared by China and lessons learned since then tells us that the virus spreads mainly from person-to-person.
The virus is not likely an airborne virus, like smallpox or measles, that circulate through the air. In an airplane, someone sitting at the back has high risk from someone sitting at the front infected with an airborne disease. But that’s not the case here.
The means of transmission are the droplets produced when an infected person coughs or sneezes.
If you are within six feet of an infected person, those droplets are the most dangerous.
Let me repeat it, the primary and major source of spread is between people who are in close contact standing within about six feet from each other. The infection spreads when the infected sneezes or coughs, and the droplets are ingested by the person nearby.
Action Number 1 to prevent or reduce spread: If you are coughing or sneezing, stay home. Cough or sneeze into a napkin, your elbow, and never into the open air. At the very least, avoid contact with others.
Action Number 2 to prevent or reduce spread: Social distancing avoids the possibility of coming in contact with droplets.
Droplets from sneezes can survive on surfaces.
A study (not yet peer-reviewed) of survival of droplets by several universities and the National Institutes of Health found:
The COVID-19 virus can survive in the air up to 3 hours, on Copper up to 4 hours, on cardboard up to 24 hours, and plastic (polypropylene) or stainless steel up to 2-3 days. [5]
It is possible to get the COVID-19 virus by touching a surface or object with the virus on it and then touching your eyes, mouth, or nose.
The CDC has said that it does not believe this is the leading way the virus spreads. But as social distancing begins to reduce the number of direct contact transmissions, surface infections will grow in importance.
Action Number 3 to prevent or reduce spread: Clean areas around you, but more importantly, practice safe hygiene. Wash hands thoroughly before touching your face.
We know that after someone is infected, they can be asymptomatic for some time before becoming ill. So is it possible for someone to spread the novel Coronavirus without being sick?
Well, the CDC believes that people are most contagious when they are sickest (most symptomatic).
The CDC goes further and says that while there have been reports of this asymptomatic spread of infection occurring, they do not believe this is the main way COVID-19 spreads.
That said, the social distancing strategy which says assume that you have the disease is the right approach.
Action Number 4 to prevent or reduce spread: Act like you have the virus, especially when dealing with someone who is in the vulnerable category (older with a medical complication).

How did we get to a global pandemic?
Although frequently identified as the source and site of patient-zero infection, the Huanan Seafood Wholesale Market (Wet market), the data presented by China CDC shows otherwise. Timeline and source follow:
COVID-19 Pandemic Timeline Highlights
First Documented Case
The first known case (retrospectively identified among the 425 early cases). The Chinese do not find a link between this case and the Huanan market. (Study)
Recent reporting suggests that the Chinese officials trying to find Patient Zero have identified cases that predate this point and are also not connected to the Huanan Market. (Public Reports)
Second Case
A second case (not necessarily identified on that date, as above). Similarly, not linked to the Huanan market. (Study)
Third Case
The third case (not necessarily identified on that date, as above). This case is the first linked to the Huanan market. (Study)
First Linkage
China CDC indicates in their study that this is the first date of linkage between Pneumonia cases and the Huanan Wholesale Market. At this point, 39 cases had accumulated, 23 linked to the market, 16 not. (Study).
Coronavirus Detected
Dr. Ai Fen, Director of Emergency Medicine at Wuhan Central Hospital, receives a lab result that contained the words: “Sars coronavirus.” She circles the word Sars and takes a photo which she shares with a former medical school classmate. That post began circulating among medical colleagues.
On the same day, Dr. Li Wenliang, a Chinese Ophthalmologist, sends a private WeChat message warning colleagues about a possible outbreak of an illness that resembled SARS, later identified as COVID-19. (Public Reports)
Public Knows
A screenshot of Dr. Li Wenliang WeChat post is leaked and circulated widely online.
The local Wuhan health authority made an official announcement saying that 27 cases of viral pneumonia of unknown cause had been detected. (Public Reports)
Huanan Market Closed
Wuhan Police announces on media that they had admonished or punished eight internet users for spreading rumors.
Huanan Seafood Wholesale Market closed. (Public Reports)
WHO informed
Dr. Li Wenliang meets with the Wuhan Police, who admonished him for “making false statements on the internet.” (Public Reports)
Several emergency protocols are activated, and the Chinese NHC informs the WHO. (Study)
US CDC Travel Warning
The Chinese CDC Level 2 Emergency response was activated. (Study)
US CDC issues a travel notice for travelers to Wuhan, Hubei Province, China, due to a cluster of pneumonia cases of unknown etiology. (Public Reports)
Novel Coronavirus Identified
The Chinese CDC announces a novel coronavirus was the causative pathogen of the outbreak. (Study)
South Korea announces its first possible case, a 36-year-old Chinese woman who had spent time in Wuhan but had not visited the market. (Public Reports)
First Fatality
The first death in Wuhan from the disease. It was a 61-year-old man who had visited the seafood market. The death was officially reported two days later by the Wuhan Municipal Health Commission. (Public Reports)
Gene Sequence Shared
China CDC publicly share the gene sequence of the novel Coronavirus; completed their PCR diagnostic reagent development and testing. (Study)
Diagnostic Reagents
China CDC provides diagnostic reagents to Wuhan. (Study)
Hero Doctor Hospitalized
Dr. Li Wenliang hospitalized. (Public Reports)
First Confirmed International
The first confirmed case from Wuhan reported outside China in Thailand. (Study)
Max. Emergency Response
China CDC raises its emergency response level to the highest (Level 1). (Study)
Wuhan Exit Screening
Strict exit screening measures activated in Wuhan for people exiting. If body temperature was equal to or greater than 37.3 degrees Celsius, the traveler could not leave. (Study)
Japan announces that a Japanese who had traveled to Wuhan is infected. (Public Reports)
Second China Death
Chinese officials confirm second death in China. (Public Reports)
The USA implements screening for symptoms at New York, Los Angeles, and San Francisco airports. (Public Reports)
Wuhan Annual Banquet
Wuhan City Government held an annual banquet celebrating the Chinese New Year, with approximately forty thousand families in the Baibuting community. (Public Reports)
Beyond Wuhan In China
The first case of infection reported in China outside Wuhan, Hubei Province. It was a traveler from Wuhan.
China CDC distributes test reagent to all provinces in China. (Study)
Human to Human Confirmed
Novel Corona – Infectious Pneumonia incorporated as a notifiable disease in the Infectious Disease Law and Health and Quarantine Law in China. (Study)
Chinese officials confirm human to human transmission of the Coronavirus. (Public Reports)
Dr. Anthony Fauci, Director of the National Institutes of Allergy and Infectious Diseases, announces NIH is working on a vaccine. (Public Reports)
First USA Confirmed Case
The first laboratory-confirmed case in the USA reported in Washington State. (Public Reports)
Wuhan Institute in China files patent to use Gilead’s Remdesivir for treatment of the Coronavirus. (Public Reports)
WHO – Not international Concern
Beijing Culture and Tourism Bureau cancels all large-scale Lunar New year celebrations. A partial lockdown of transport in and out of Wuhan and neighboring cities Huanggang, and Ezhou Huanggang enforced. (Public Reports)
An emergency committee of WHO says Wuhan Coronavirus does not yet constitute a public health emergency of international concern. [6] (Public Reports)
USA Increased Travel Warning
US CDC changed its travel guidance several times to an eventual Warning – Level 3, Avoid All non-essential travel to China. (Public Reports)
WHO & China Meet
China President Xi Jinping meets with WHO Director-General, Tedros Adhanom, in Beijing, agreeing to allow a team of international experts to visit China to investigate the outbreak. (Public Reports)
US Task Force
Zeng Guang, the chief epidemiologist at the Chinese Centre for Disease Control and Prevention, said in a national television broadcast that the eight people punished by the police should be held in “high regard.” [7] (Public Reports)
White House announces a new task force to monitor and help contain the spread of the virus. The task force will also be responsible for providing accurate and up-to-date travel information to the American public. (Public Reports)
WHO – Is International Concern
The first confirmed case of person-to-person transmission in the USA. A woman in her 60’s from Illinois diagnosed with Coronavirus after returning from a trip to Wuhan infected her husband, also in his 60’s. (Public Reports)
Italy closes all air traffic to and from China. (Public Reports)
WHO declares the Coronavirus outbreak is a health emergency of international concern. (Public Reports)
US Denies Entry
Dr. Li Wenliang posts on social media details of his WeChat posts and the interactions with the Wuhan Police. (Public Reports)
Italy declares a state of emergency. (Public Reports)
The USA announces it will deny entry to foreign nationals who traveled to China in the previous 14 days. Citizens will be allowed in but quarantined. (Public Reports)
Tighter Cremation Rules
China’s National Health Commission requires the cremation of victims of Coronavirus at the nearest facility. No farewells or other funeral activities involving the corpse are allowed. (Public Reports)
First Death in Philippines
First death from the Wuhan Coronavirus reported in the Philippines. It was a 44-year-old Chinese man who arrived from China. (Public Reports)
China Questions US Policy
China’s Foreign Ministry Spokeswoman, Hua Chunying, accuses the US Government of inappropriately reacting to the outbreak. She said: “Even American media and experts doubted the government’s decision, saying that the US government’s restrictions on China are precisely what the WHO rejects, that the US is turning from overconfidence to fear and overreaction, and that banning the entry of foreigners who traveled to China in the past 14 days is suspected to be violating civil rights instead of reducing risks of virus spreading,” [8] (Public Reports)
Hero Doctor Dies
Dr. Li Wenliang died of the virus. [9] (Public Reports)
First Foreign Fatality in China
The first confirmed death of a foreigner in China of COVID-19. It was a 60 year old US national. (Public Reports)
Xi Jinping seen in public
China President Xi Jinping is seen in public wearing a protective mask and having his temperature checked in Beijing. (Public Reports)
A Name – COVID-19
The WHO names the Coronavirus COVID-19 (Public Reports)
US CDC Kit Fails
USA CDC announces that a diagnostic kit it developed does not work due to a problem with a reagent. (Public Reports)
First Fatality in Europe
A Chinese tourist tested positive for the virus, dies in France. It is the first COVD-19 death in Europe. (Public Reports)
Conspiracy Theories Abound
Wuhan Institute of Virology releases a statement that no members of the institute were infected. The announcement was in response to allegations that Patient Zero was a research student at the institute. (Public Reports)
New Cases Outside Exceeds New in China
NIH announces that trials on antiviral drug Remdesivir start at the University of Nebraska Medical Center in Omaha. (Public Reports)
Italy’s Lombardy region begins the complete lockdown of several towns and villages. (Public Reports)
Number of new cases outside China exceeds the number of new cases in China (Public Reports)
US VP Leads Task Force
US Vice President Mike Pence appointed to head up the Task Force and lead the US Government response to COVID-19. (Public Reports)
First USA Fatality
First COVID-19 death in the USA, a patient infected in Washington State. The Governor declares a state of emergency. (Public Reports)
The USA bans travel from Iran and raise travel warnings to Italy and South Korea. (Public Reports)
State Emergencies Begin
Florida declares a public health emergency. Kentucky, Maryland, New York, Oregon, and Utah declare states of emergency in the next few days. (Public Reports)
EU Goes to High Risk
The European Centre for Disease Prevention and Control increases the risk level for people in the Union from moderate to high. (Public Reports)
Italy Locks Down
Italian Prime Minister, Giuseppe Conte, announces lockdown of Italy. (Public Reports)
COVID-19 is a Pandemic!
US Government announces travel restrictions from Europe. (Public Reports)
WHO declares the COVID-19 outbreak to be a pandemic. (Public Reports)
Why testing is a tool in the fight, but an incomplete solution.
You have seen a variety of tests being used across the world. First, there were temperature tests, then later reagent based or more complex tests. All of these tests had a role to play, but how effective were they?
Temperature Testing
A core temperature spike is a useful method for identifying someone who may be symptomatic with a high fever.
However, the temperature test has a very high rate of false positives and false negatives. Meaning this test does not differentiate people who have a high temperature from something like regular influenza. And, more importantly, not having a high temperature does not mean you don’t have the Coronavirus.
Temperature testing is a useful screening tool, but not a complete solution.
PCR and Antibody Tests
The available diagnostic test in the USA is a Polymerase Chain Reaction (PCR) test developed by the CDC. Similar to the test used for detecting HIV, the Coronavirus PCR test looks to identify genetic material called RNA from the Coronavirus.
The early PCR test is unpleasant. It consists of a health care worker, in protective gear, using a long Q-tip inserted through the nostril to swab the back of the throat. The swab goes to the nearest approved lab for testing, and the health care worker must change their gear before performing another test.
Early on, those swabs went to the CDC, creating a natural logistic time lag. Once at the CDC, low volume testing processes meant low throughput and resulted in longer than necessary cycle times.
Since the early stages, the US Government and the CDC have worked diligently on transforming the process. The new public-private partnerships completely redesigned the supply chain for COVID-19 PCR tests incorporating higher throughput automation and moving labs much closer to the testing sources. Expect to see further improvements in this area.
Other PCR methods have been devised, such as saliva samples, a liquid sample from the lower respiratory tract, or stool samples. Each PCR test type has its benefits and challenges. But all follow the same process after collection, ending up in a testing lab with a search for the Coronavirus RNA.
Some countries, like China, have developed an antibody test, which works on blood drawn. With antibody tests, the testing process requires mining the collected sample for antibodies specific to the disease.
Whether a PCR or Antibody test, the sample takes hours to run in the labs, meaning results could be ready within a day. That is the case until we develop and rollout rapid form tests which will deliver tests within hours. [10]
Testing Challenges
There are two challenges with the state of testing.
The first is the problem of a false negative. Because the amount of virus produced by the body can change from day to day, so too can the results. Dr. Chiu says: “The take-home message is that a test that looks at a single time point is not sufficient to rule out infection,”
The second challenge stems from testing being akin to searching for a “needle-in-the-haystack.” In South Korea, where symptoms indicated testing, there was a 3 to 4% confirmation of Coronavirus. In the USA, the early results have been 1 to 2%.
That means, in the USA, we are testing 50 to 100 people before one Coronavirus infected is found. Keep in mind that the testing so far has been where patients have symptoms and are recommended for testing by a medical professional, we are getting meager confirmation rates.
Imagine opening up testing for any American who wants the test!
Testing is a helpful tool but an incomplete solution.
The Bottom line on Testing.
Our testing process in the USA was not set up for this kind of Pandemic. We are fortunate that the red tape was cut and innovations in testing are showing up. We need some serious improvements in our diagnostic testing capabilities.
We need everyone who shows symptoms to act like they have the virus.
We need anyone who shows the symptoms and is most vulnerable to seek medical care.
They may need specialized care regardless of the infection, and their medical professional can determine the importance of the test.
The worst-case analysis should be for scientists and policymakers only.
You have seen the headlines.
75% of the population will become infected. Hospitals will be overwhelmed. And on and on, reflecting a worst-case scenario of possibilities.
To what end?
We most certainly don’t want the public to act like the worst-case is likely. That’s what causes the emptying of food shelves, the silly hoarding of unrelated basics like toilet paper, etc.
So why would respected media be peddling stories about the worst-case scenario, other than to support those who profit from panic?
Look, every emergency management team does scenario planning. Typically, there will be the best case, worst case, and most likely scenarios. Thoughtful organizations will run many simulations to reach consensus on the likely scenario. Any good emergency plan will require the managers to think through what metrics they need to track to ensure they are trending to the likely scenario. They will also identify breakpoints that indicate when its possible to get worse than the likely scenarios. Most importantly, they will develop a series of contingency plans around what to do should things begin to get worse.
All of that is in the domain of those managing the emergency. But all emergency managers know that they must do everything possible to make the likely scenario or better occur. Wise emergency managers will hedge their bets and paint a scene worse than their likely case. So imagine what happens when you take a conservative forecast and layer even more pessimism by focusing on the worst outcome.
There is no public good derived by having the public confronted with the worse case when there are so many other more likely scenarios that are less dangerous.
Panic is a killer in emergencies. Avoid at all costs!
Real criminal COVID-19 behavior – reckless endangerment!
A UK citizen diagnosed with Coronavirus and advised to remain in quarantine, boards an Emirates airline flight from Kochi to Dubai.
A Google employee tested positive for Coronavirus after he returns to India from Italy. His wife, required to be in quarantine, manages to evade authorities. She gets on a flight to Delhi. From there, she gets on a train to her parents’ home in Agra, several hours away. Officials faced resistance when they went to her house, including a denial by her father that she was there. She was moved to isolation after a magistrate intervened.
A man with symptoms takes the test for Coronavirus in New York. He had not received his results when he gets on a JetBlue flight to Palm Beach. He learns mid-flight that his tests are positive.
There have been many similar reported cases around the world.
The guideline is simple. If you have any symptoms, act like you have Coronavirus.
People who have a respiratory disease, especially those diagnosed with Coronavirus, have no excuse for avoiding a quarantine.
This behavior is reckless endangerment!
They should be prosecuted.
What is the problem with the case examples given at the beginning?
At the start, I gave three examples of the kinds of readings that prompted me to put this article together. Let me detail what exactly was the issue with each.
Second-guessing the decision-makers
In the first example, my friend, who is well educated and frequently very thoughtful, asserts that a policy decision to shut travel from Europe is misguided.
We see this frequently, sideline quarterbacks questioning the coach’s call.
Here is what I know.
Decision-makers, especially in an emergency, have a lot more and better information than I have. And unless I have a unique specialty that allows me to analyze that data and identify anomalies they can’t see, we ought to give them the benefit of the doubt.
Dr. Li Wenliang was a professional with better facts and was appropriately in a position to question the official story in China.
My friend, like the average American, does not have either the data or the expertise to weigh in on policy decisions.
30 of 35 infected clusters investigated in the USA were traced back to travelers from Europe. That was the basis for the decision.
Regardless of your political or personal inclination, in a crisis, if you are not a subject matter expert, then ask for clarification; don’t assume stupidity.
Politics and Pandemics are a terrible mix
Yes, I know many of us are wedded to a political ideology.
I wrote a piece here recently about politically-obsessed friends and how to deal with them.
In this example, a noted opinion writer for a publication that has been on the other side of the President since his election, suggests the pandemic will be worse for Republicans than Democrats. She argues that Democrats will follow the guidelines of authorities and the media, and are more likely to practice social distancing and other necessary behavior than those cavalier Republicans.
This ideological lens is so wrong on so many levels that it’s mostly apparent to any reader.
My bottom line? It’s most useful to stick to real questions of meaningful value.
Avoid politics in a Pandemic.
Understand the right goals to get clarity on the right choices
The third case was annoying to me for the simple reason that the author made some simple logic mistakes and then further compounded the error by advocating an unworkable alternative to the current strategy.
But as I dug further, I realized there was a more fundamental disconnect between descriptions by the authorities of what they are trying to accomplish and what they can achieve with what they are doing.
Let me go through this slowly, as there are a lot of thoughts here.
The author was focusing on the dangers of a social distancing strategy by prolonging the pandemic.
He focused on the damage to the economy due to an extended social distancing strategy and economic slowdown or shutdown.
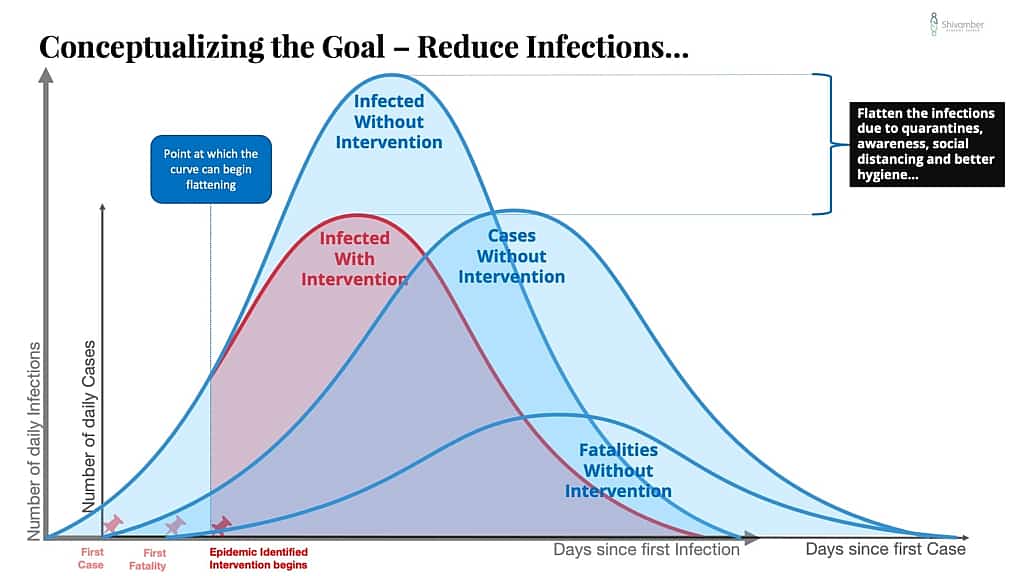
The author used the charts shown frequently by the CDC of a pandemic curve and the flatter version (you know the one that Dr. Anthony Fauci uses all the time). It’s a chart from the CDC Pandemic playbook, which has been around a long time and most recently updated in 2017.
The author said something that stood out to me: “You notice the number of cases doesn’t change (the area under the curve).”
This constant number of cases is the assumption that results in the flatter curve spreading out significantly longer.
Why should a strategy to prevent or reduce the spread in a virus result in the same number of cases as allowing the pandemic to take its natural course?
It shouldn’t.
Like a shiny object, the author’s suggestion to develop an alternative strategy of smart quarantining temporarily distracted me. This proposed strategy is based on testing and assumes that the technology to test millions of individuals quickly is available.
I have already addressed the issues of testing above, so this recommendation was a non-starter.
Testing is not fool-proof, nor is it available for everyone in the population.
A single false-negative could result in infectious spread to a previously safe group and require retesting, ad infinitum.
The author did make one suggestion that was very interesting in his smart quarantine proposal that does make sense. He suggests quarantining all seniors over 60, nursing homes, and the like.
The strategy employed by the task force seems to have incorporated some of this good suggestion, particularly as it relates to nursing homes.
Perhaps we should consider a more forceful declaration of quarantine for those over 60 with a medical condition?
Conceptualizing the Strategy
Despite the short temporary distraction, I kept returning to the chart and the concept it was communicating.
Then it dawned on me that the chart was wrong.
It does not reflect what likely happens at all.
Like most conceptual charts, the authors though to communicate the salient points, but did not pay attention to the details of the display and what they meant. Let me explain and try to tease out the subtle differences that will make in how the strategy works.
Here is the chart used by the CDC and the US Department of Health and Human Services.
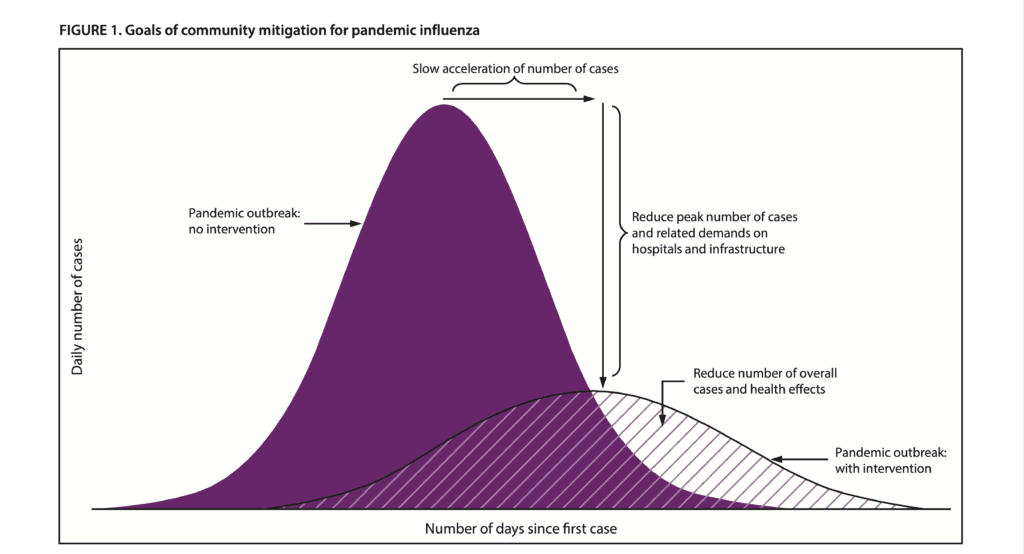
It is found on page 3 of the report titled Community Mitigation Guidelines to Prevent Pandemic Influenza – United States, 2017 [11]
The curve with the higher peak is the Pandemic outbreak with no intervention.
The lower curve chart is the pandemic outbreak with intervention.
The lower curve on the CDC chart is conceptually incorrect and impossible to achieve.
Why?
It’s impossible because the flatter curve shown begins later than the no intervention curve.
Those two curves have to be the same at the beginning.
In every epidemic, there is a period after the first case where cases are increasing before any early warning system indicates there is a pandemic.
There is typically no intervention until that stage.
To help you understand this better, I had to go to the drawing board and re-visualize the curves. Here is my version.
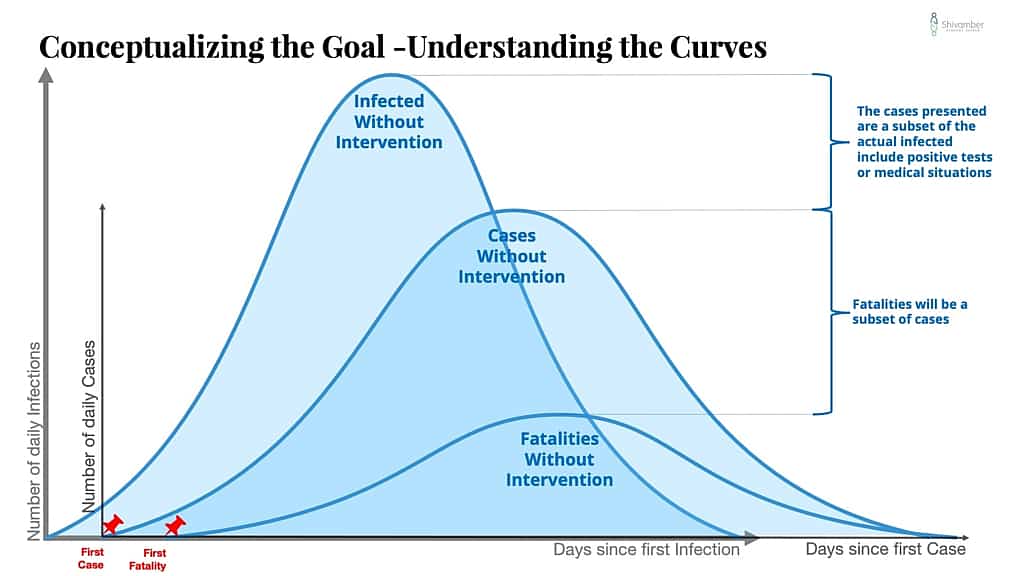
Please note that I made some distracting, but hopefully useful additions. I wanted to highlight the overall view of what is happening as a virus becomes a pandemic.
First, we need to understand that before the first case becomes a medically identified situation, there is a virus in the wild that’s percolating along.
My chart starts with the first infection!
I have added a layer to the chart to the left of where the CDC Chart begins, to represent the beginning of infections and a curve that shows hypothetical infections. The real number of infections are never all known to the health care system.
As the infections spread, there is an eventual condition that triggers a medical visit.
I have placed a pin on that date. This is where the traditional CDC chart begins.
Medical cases are always a subset of infections and are a lagged observation. Depending on how sneaky the virus is, it could be a while before someone has enough complicating symptoms to visit a medical center. And then they will have to trigger some tests to identify the underlying virus.
That means that the medical system information on the virus will always be behind the curve.
Medical cases, and any fatalities, will continue to pile up at some proportion of infections, depending on the specifics of the viral effect.
Important Note: On the case chart, there will be a moment in time when the cases will spike due to a change in counting source. The early cases will come from medical situations. Later there is typically a switch to public or external testing. At this point, people who don’t show symptoms or who don’t necessarily show up for medical care will be identified as cases. This spike in cases does not mean a similar spike in fatalities.
At some point, the health officials will gather enough evidence to classify the situation as an epidemic.
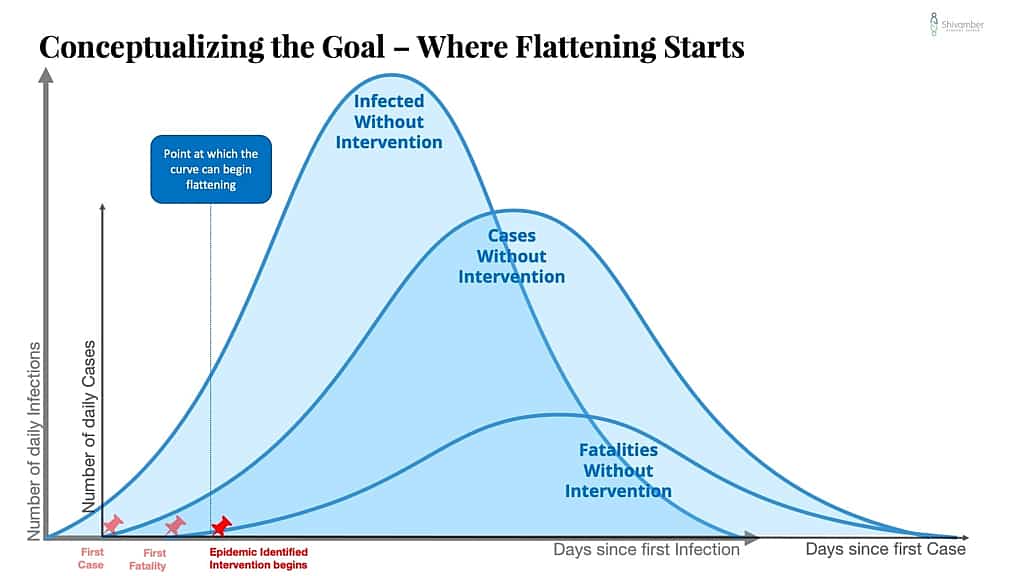
Until then, there can be no flattening of the curve.
It is only after the early warning triggers that useful intervention can begin to flatten the curve.
An aside. After the SARS epidemic, China redesigned its early warning system. It should have triggered at the end of December upon the coronavirus lab result. However, that was not what happened. Real interventions did not take place until much later.
The later the early warning system triggers, the further up the curve one will go before flattening can begin.
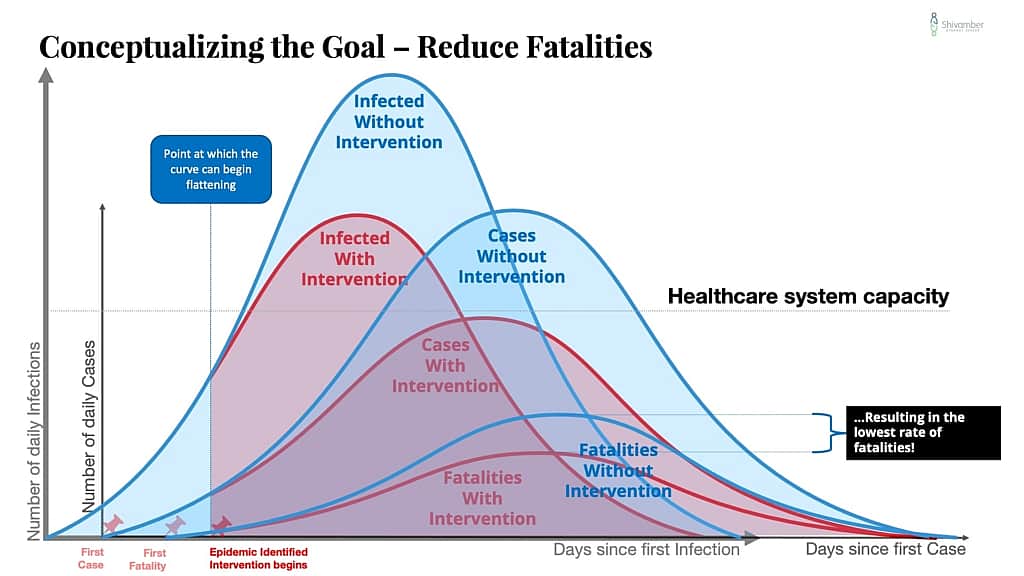
In this series of charts, I show conceptually what happens with an effective intervention that substantially reduces the rate of transmission of new infections.
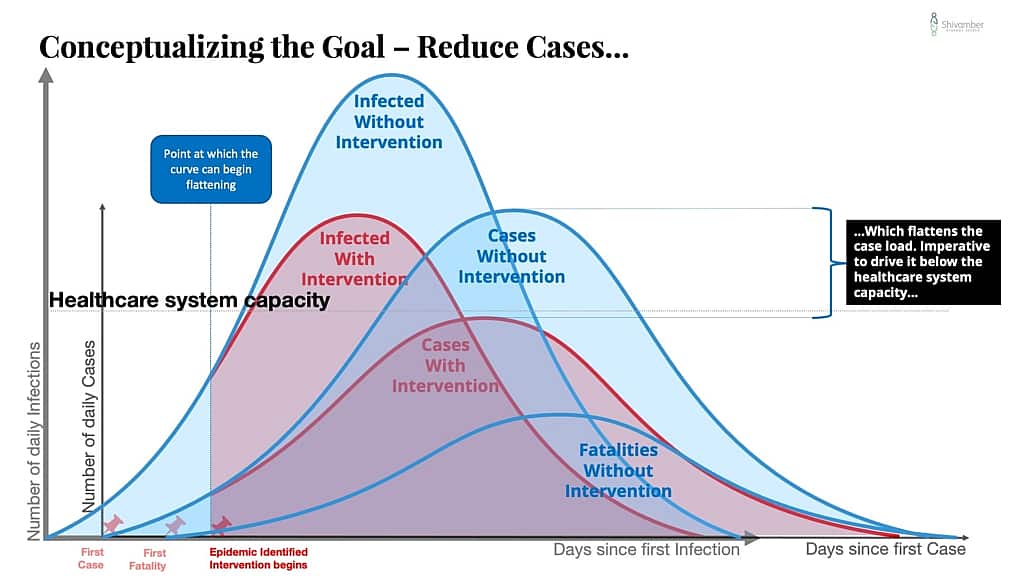
One way to get a flatter curve is to create a better early warning system. The result is that you identify the problem earlier and lower down the start of the curve.
The second insight is that all else being equal, the pandemic has a natural life cycle.
Use this thought exercise. Assume the worst-case pandemic without intervention. That would be a situation in which everyone in a population is introduced to the virus quickly, and the community achieves herd immunity. That curve will be high and thinner.
We can’t do that with COVID-19 because of the high mortality, but the thought exercise is essential in understanding how the curves change and what causes them to change.
So in a naturally occurring pandemic with no intervention, people are infected, treated, recover, or become fatalities in a curve that is somewhat lower peak than the worst-case thought exercise, and also flatter base.
The width of that base represents the time for the virus to work its way naturally through the community. Let’s call it the natural duration of the pandemic.
Now, let’s extend that thought exercise to the best case. Let’s assume that at the early warning trigger, everyone stood still, meaning no more social interaction, and no more transmission occurs. The case curve will continue to increase for some time as all those already infected but not symptomatic are identified, treated, recovered, or become fatalities.
This curve will climb further to the right of the early warning point, but flatten out quickly and drop quickly for about the life-cycle of the virus. With COVID-19, this would be about 12.5 days at the 95% interval. To be extremely cautious, one should use the most prolonged incubation period and assume that base, after early warning.
If there are no reinfections, then the curve should drop to no new cases after that interval. This best-case curve is a significantly lower curve and a narrower base than the no intervention curve.
So a well-executed strategy to prevent or reduce the spread of COVID-19 or any pandemic should result in a curve that fits between the best case and the natural case (lower height and narrower base).
What keeps us from a resulting curve that is lower and thinner than no intervention curve?
Here are a few possibilities:
- A mutating virus.
- Reinfections. Newly infected additions to the community.
- Uncontrolled leakage. Primarily due to an inability of the community to implement social distancing and suitable hygiene measures.
- Catastrophic failure. A health care system overwhelmed with cases greater than its capacity to operate effectively.
The strategy to prevent or reduce the spread of COVID-19 must include contingency planning for these and other possibilities.
Policy decisions must force the new curve below the crisis capacity of the health care system, and the system capacity raised.
There are a lot of smart people laser-focused on this problem. I hope that the misinformation driven panic and the emotional tendency to rely on stories does not create missteps.
Why we need testing to get better fast.
Even if a community has done a great job of flattening their curve and eliminated the virus, we live in a connected world that allows for the reintroduction of the virus.
The problem here are the cheaters or travelers from those areas that are still feeling the effect of the pandemic.
I have discussed the cheaters earlier in this article and will address them again with the lessons learned below.
Managing travelers is the most critical piece to solve in ensuring the community strategy holds. You can see that China, which has largely shut down the virus in China has had to recently shut down travel from locations that are now in the midst of their struggles. That is necessary to ensure that China doesn’t get reinfected.
After the 9/11 terrorist attack, we saw a dramatic change in passenger screening. This will be necessary to reopen borders, or everyone will have to wait until the last community is free of COVID-19, at significant other penalties.
For a screening system to work will require broader use of thermal measurement systems and significant improvements in the testing approach.
Testing will have to be much more immediate, and much more accurate.
A Hidden Benefit?
There could be some good news in all of this.
The CDC has identified from the China experience and continuing results that the Coronavirus is most dangerous and highly fatal to the elderly with medical complications.
In the fight to stave off infections to the most vulnerable, the decisions to focus on preventing or reducing the spread are the right priorities.
Social distancing and asking anyone with symptoms to act like they have the infection are potent tools. These actions may very well result in saving lives that be otherwise lost, not just to Coronavirus.
Here is how that works.
Everyone tested, who presents themselves with symptoms, is suffering from a respiratory disease. All respiratory diseases, such as influenza, are dangerous and sometimes fatal to the elderly, particularly those with complications.
Through social distancing and other measures, we are, in effect, not just preventing or reducing the spread of Coronavirus. We are also preventing or reducing the spread of all other contagious respiratory diseases.
The hidden benefit is that while these new behaviors persist, we may see reductions in many influenza or other respiratory-related deaths!

Lessons Learned
During a crisis is not the right time for blame seeking or sideline second-guessing the emergency managers.
It’s never valuable to stand at the edge of the pool and shout instructions to the drowning swimmer.
And, it is equally a waste of time to be shouting corrective measures to the lifeguard who has jumped in to help.
Get a line, a life jacket, call an ambulance. Figure out what you can do to help.
Some will never be able to observe a situation without falling into the trap of assigning blame or second-guessing the observed actions taken.
But in an emergency, that kind of behavior gets in the way of getting the crisis resolved quickest.
The bane of emergency management is an abundance of options, and the ensuing analysis that keeps one from making decisions.
Good emergency management organizations have structured checklists, processes to review alternatives, and approaches to facilitate timely judgments.
Observers, without relevant expertise, will never have the same information as the emergency managers. Your suggestion might be useful, but it may do more harm than good.
There will be time for you to return to your interest in assigning blame.
Just not during the crisis.
Jump in and focus on what you can do to help the strategy succeed.
China could have done better.
China understood the need to lock down Wuhan, and then later to lock down other cities to avoid further spread.
Each lockdown was late, resulting in infected beyond the locked-down area. However, each lockdown was effective in dramatically reducing further spread.
But the Chinese did not lock down China.
At the very least, they could have implemented a screening process for passengers leaving China.
This move would have likely been late and not wholly fool-proof, but it could have significantly lowered the number of infected leaving China, leading to the global pandemic.
WHO could have done better.
On January 23, 2020, an emergency committee of the World Health Organization (WHO) says Wuhan Coronavirus does not yet constitute a public health emergency of international concern.
Based on the discovery that China was dealing with a Coronavirus, the only reason it is not of international concern is if WHO assumes China can control the virus to stay within its border.
Cases had already shown up beyond Chinas borders and reported in several countries.
I can see no justification for such an assumption by the WHO.
Even were WHO to make such an assumption based on concrete reassurances from China, at the very least, WHO should guide China to demonstrate steps taken to avoid the spread beyond its borders.
On January 28, the Director-General of WHO meets with President Xi Jinping. They agree for the WHO team to visit China to investigate.
On January 30, WHO declares a health emergency of international concern.
The WHO team arrives in China on February 10.
Why wasn’t that team ready January 28 or immediately after that?
WHO was an abject failure at best, or may have even exacerbated the effects of this pandemic.
Partial barriers don’t block; they only slow.
The Chinese partially blocked departures from Wuhan early, but many continued to travel out.
Italy blocked flights to and from China early. Even earlier than the USA. But the open Schengen borders meant infected travelers rerouted and ended up in Italy a different way.
The USA also instituted early screenings. That decision likely dramatically lowered the influx of directly infected travelers. However, those travelers continued to pour into other destinations, mainly Europe, and infected Europeans unwittingly spread the infections.
Which leads me directly to this last lesson:
Always plan for rule-breakers.
Rule breakers are brilliant at doing stupid things.
Iran instituted a flight ban at the same time as the Italians, earlier than the USA.
However, it’ appears that one Iranian carrier owned by the Iranian Revolutionary Guard Corps continued to fly to and from China despite the ban.
Further, it seems that Chinese, among them infected, continued to travel to Qoms where there is a massive Chinese infrastructure project
How does one explain an individual confirmed infected with COVID-19 continuing to move amongst others?
Whenever we create barriers, a lot of creative juices go into figuring out alternative ways to get around the obstacle.
With something as the life and death consequences of COVID-19, we need to understand what rule-breakers are likely to do and ensure we cut them off.
Our strategy to prevent and reduce the spread of COVID-19 is the right strategy; we all need to do whatever it takes to make it work.
Improvements needed for future
- Continue to innovate on improving the early warning system. WHO failed. USA CDC was early, but it is a leader and should have been more vocal.
- We need to reinvent field diagnostic testing. Good to see the public-private partnership started here. It has to accelerate.
- The medical supply chain is fragile. For the USA, its current structure could pose a national security risk. Critical unreliable dependencies must be better understood, managed, and eliminated over time.
- The economic/political considerations appeared to obfuscate fact-based and clinical decisions. How do we better balance national interests and extra-border impacts?
Postscript
If you made it to the end, thank you. My apologies to you for the long screed. This burst of curiosity is what happens when I find myself with more free time than I had planned. Stay safe!
Benchmarking Fatalities
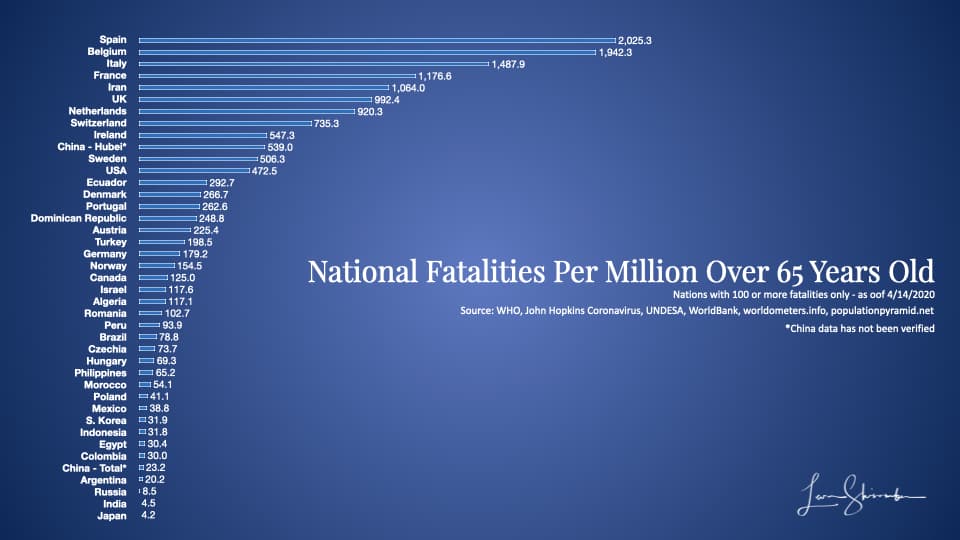
I was curious if we could understand anything by looking at the relative fatality rates.
I had seen the fatality rates by country but then the caveat was always that the virus really affected the elderly much more than the young. And the statistics show that the vast majority of fatalities are indeed among those 60 years or older.
Fortunately there is data available for the population of each nation and the proportion of the population over 65 years old.
Using this data and the fatalities by the nation on Johns Hopkins Coronavirus real-time site, as of 3/23/2020 9:20 pm EST the following is what the chart looks like for the top fatality rate among those primarily at risk (population 65 years and older):
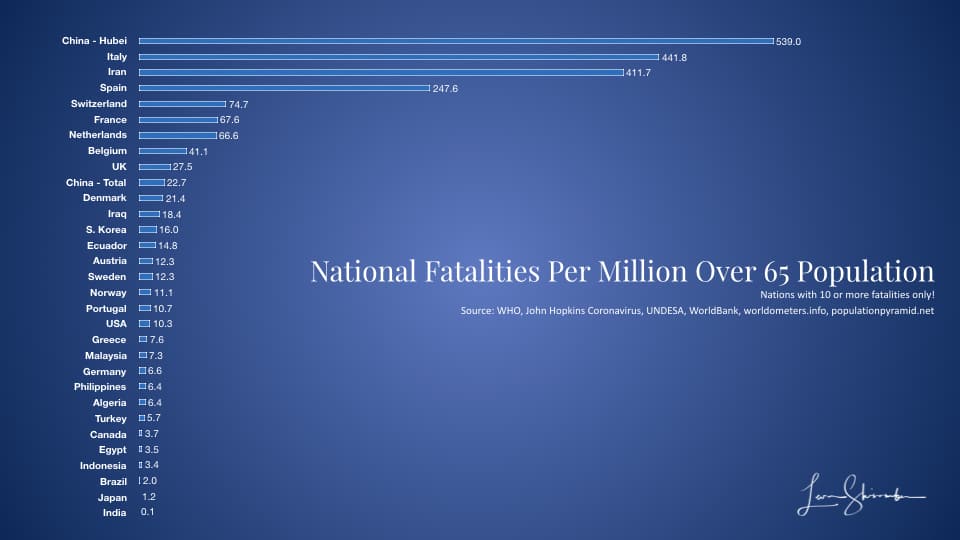
As of 4/14/2020 11:20 am EST. the following is what the chart looks like for the top fatality rate among those primarily at risk (population 65 years and older), but including those countries with 100 or more fatalities:
Sources:
[1] https://www.breitbart.com/clips/2020/03/15/wapos-jennifer-rubin-there-will-be-less-democrat-coronavirus-deaths/
[2] https://cliffmass.blogspot.com/2020/03/panic-and-coronavirus-is-there-is.html
[3] https://www.nejm.org/doi/full/10.1056/NEJMoa2001316
[5] https://www.medrxiv.org/content/10.1101/2020.03.09.20033217v2.full.pdf+html
[7] https://www.scmp.com/news/china/society/article/3048283/politics-may-have-stalled-information-wuhan-coronavirus-crisis
[8] https://www.cnn.com/travel/article/coronavirus-us-travel-restrictions-monday/index.html
[10] https://www.livescience.com/how-coronavirus-tests-work.html
Just A Detour…
I had some free time and could not escape from the curiosity induced by the question of whether the opinion writer, discussed in the example above, was even accurate.
Disclaimer: This is not intended to be scientific, or even an analysis that would be of interest to me. But I wanted to lay out an analytical approach if it was a serious question.
How could you figure out the impact of COVID-19 on Democrats versus Republicans?
To most effectively model the impact by parties, one would have to build a model and run varying assumptions of what happens in each case.
Below is the starting point of one such approach. The point is with proper statistical modeling and analysis; one could have a much more fact-based conversation of impact rather than the typical broad over-generalization.
This analysis should not be taken too seriously as it is just a simple exercise, which would require a healthier dose of precision to be useful. But you can get a sense of how to approach the problem.
First, the most affected will be seniors with underlying conditions. We don’t have demographic data to that level of detail, but we do have some data without underlying medical conditions.
The Pew Research Center report published on March 20, 2018, titled “Trends in party affiliation among demographic groups,” provides us some useful data about the proportion of each generation by party affiliation. Statista provided the numerical count of each group, and the Chinese CDC provides some data about death rates by age group.
What did I find?
By using the PEW survey where individuals identify as either Democrat, Independent, or Republican, we could estimate 31.2% of fatalities would be Democratic versus 30.4% Republicans.
Using the second survey where individuals identify as Democrat or Democrat-leaning versus Republican or Republican-leaning, we could estimate 42.5% of fatalities would be Democrat or Democrat-leaning versus 44.5% Republican or Republican-leaning.
So this exercise was mostly inconclusive as one analysis says more democrats while the other says more Republicans.
That said, I lean toward agreeing with the commentator that Republicans will see more challenges from the COVID-19 pandemic, but not for the same reasons:
- The most affected group, The Silent Generation and the Greatest Generation, are the only demographic group where Republican affiliations outstrip Democrats.
- The younger the demographic group, the higher the Democratic affiliation gap over the Republican affiliation.
You get the idea of how to go about doing this.
Apologies for the detour, but that’s how one can approach the question empirically, by using the probabilities and sizing of different groups.
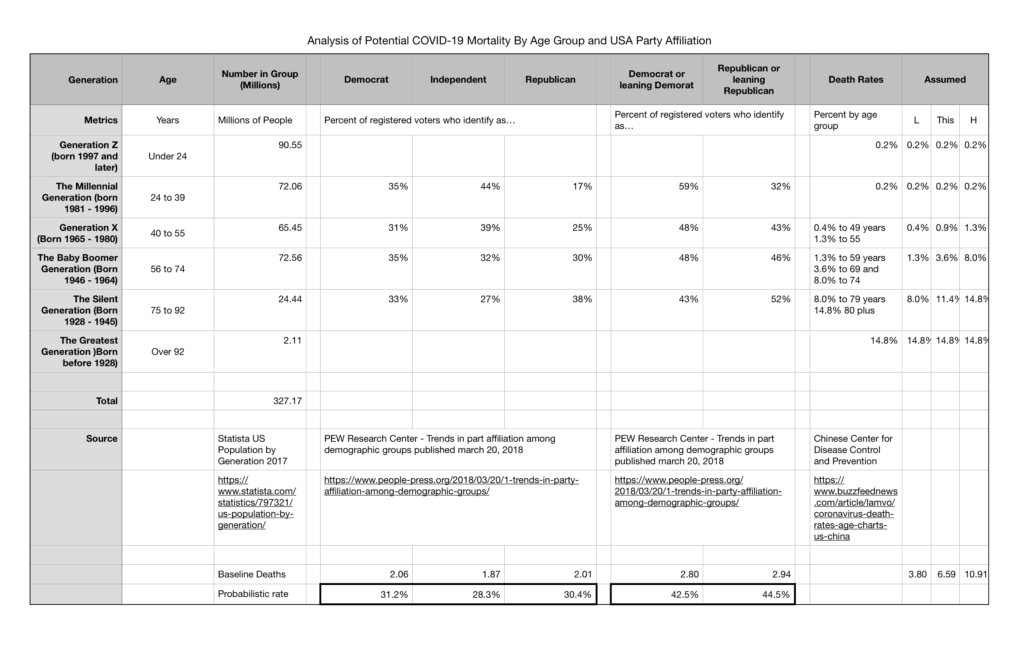
Here is a link to my starter model to get you started:
https://docs.google.com/spreadsheets/d/1RDZh1SvTGccKC_VhWyp9gk57ck_kmjnAcDFyJBb5f-c/edit?usp=sharing
[11] https://stacks.cdc.gov/view/cdc/45220
https://coronavirus.gov
https://cdc.gov